In what might be a world first, the Frank H. Netter School of Medicine in the US has fully integrated ME/CFS into its curriculum.

The training program was developed by Dr Howard Andrew Selinger, a family physician and Chair of Family Medicine at the school. When asked how he became involved with ME/CFS, Selinger replied:
“Well, I have to be honest and say that for the first thirty-five years I knew nothing about it, like most family physicians, I think. That is the norm, unfortunately. I became involved when I was approached by a lovely woman who struggles with it, and is in her eighth decade of life, and we were blessed with an endowment for my chair, and the ask that came with that endowment was to please develop a curriculum so students of medicine can hear about this, understand the fundamentals, and enter their clinical careers so that they can build on that knowledge base.”
When asked how the training was received by students, Dr Selinger replied that the students were grateful, receptive and open-minded. What resonated most for them was having the opportunity to hear patients describe their experiences live and in their own words, either in person or over zoom.
The curriculum
Students receive training on ME/CFS in each of the first three years of their studies, with the option to build on that knowledge in the fourth year with a clinical placement.
Year 1:
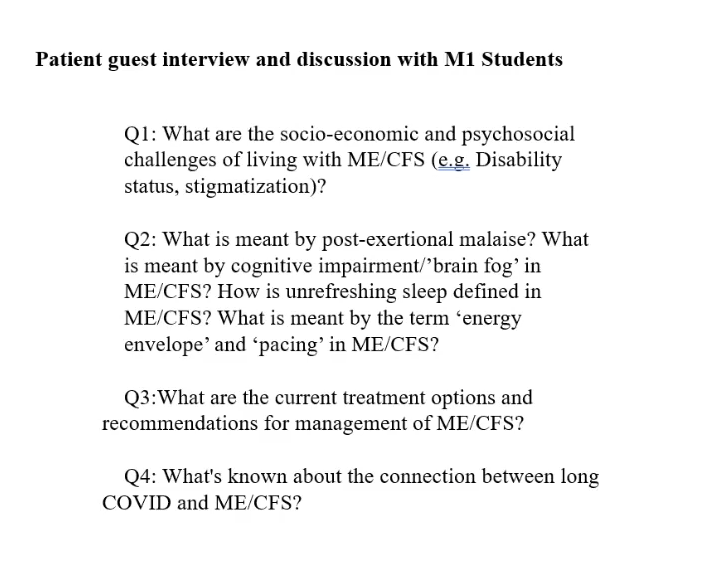
Students spend two hours hearing from two patients with ME/CFS and their families, who describe what it’s like to live with the condition. Students are also introduced to the stigma and knowledge gaps which exist in the medical world.
Year 2:
Students interview and examine a patient and come up with a set of possible diagnoses, one of which is ME/CFS. The students then make a case presentation.
Year 3:
Students receive a detailed presentation covering the latest scientific and clinical knowledge on ME/CFS. Dr Selinger provides a simplified version of this presentation in the video below.
Year 4:
Students have the option to do a four-week clinical elective at the Bateman Horne Center, a center of excellence for ME/CFS research and treatment.
Dr Selinger describes the training program in detail in the video presentation below.
